From expert to patient
It is with great sadness that we share the news of Dr. Tresa Roebuck Spencer’s passing in September 2024. Dr. Roebuck Spencer was a passionate and dedicated advocate for neuropsychology at the national level. Her loss is deeply felt by the National Academy of Neuropsychology (NAN) community. A board-certified clinical neuropsychologist and former NAN president, Dr. Roebuck-Spencer worked in Texas, Louisiana, Florida, and Washington, D.C. She authored more than 70 peer-reviewed publications and book chapters on topics such as traumatic brain injury, rehabilitation, and computerized neuropsychological testing. In the final years of her life, Dr. Roebuck Spencer faced her own medical challenges after being diagnosed with glioblastoma multiforme (GBM) in October 2020. She bravely navigated treatments that included four brain surgeries, three clinical trials, and multiple rounds of radiation and chemotherapy, all while continuing to educate others about her journey. In recognition of Glioblastoma Awareness Day on July 19, 2023, BrainWise Managing Editor Matt Villano interviewed Dr. Roebuck Spencer about her experience. The following is an edited transcript of their conversation.
BrainWise: Take us back to the beginning. How did your experience with GBM begin?
Dr. Tresa Spencer: On October 13, 2020, I was in my office working, and I started to feel funny. I had no symptoms or problems prior to that point, I was just living my everyday normal life, as a working mom, traveling frequently while establishing my fast-growing private practice. I’m a bit of an over-achiever, so it was not uncommon for me to start my day with a Camp Gladiator workout and then fall asleep with my laptop in my lap writing reports. So, I was in my office, and I started to feel funny. I had the wherewithal to call my neighbor who lives right down the street and say, ‘Can you come check on me? Something’s not right.’ I was dropping things out of my left hand and kept mistyping my passwords. I started thinking, ‘Am I having a stroke? What’s happening to me?’ When my neighbor arrived, I was walking around my office, doing a neurological exam on myself. I was raising my eyebrows, sticking out my tongue, and having her look at my pupils. I was walking back and forth to test my balance. I knew something was wrong but didn’t know what. It was a surreal experience, as you might imagine. We called our other neighbor who’s a physician, for her advice, because I was starting to feel dizzy at that point. Then we went to the ER. I made sure to take my work bag, thinking I’d be home within a few hours. As we were driving to the ER, my voice sounded strange, and I continued to assess myself, trying to make sense of what was happening to me. I instructed my neighbor what to tell the ER triage nurse, because I knew if I got there within a certain amount of time, they could give me [tissue plasminogen activator, or TPA,] a particular medication that helps lessen the effect of stroke. So, I told her, ‘Tell them my symptoms started at 10:00 a.m., and that we’re getting here within an hour. They can still give me TPA.’ I wasn’t only assessing myself, but I also was thinking about how to give an accurate history, and what my treatment plan would be. When we got to the ER, I started to explain my symptoms, and I passed out.
BrainWise: What happened next?
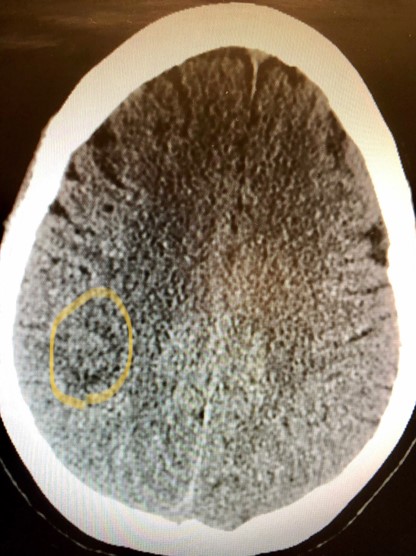
Dr. Spencer: My next memory is of waking up in an exam room and my neighbor staring at me with the biggest eyes I’ve ever seen. I asked, ‘What’s going on?’ At that point, I was confused. And she looked at me and said, ‘Tresa, you just had a seizure.’ And I said, ‘Well, what kind of seizure?’ I immediately went back into clinician mode. And she said, ‘How do I know what kind of seizure?’ So again, being a clinician, I said, ‘Well, describe it to me,’ because that’s what I would say to a patient. And she said, ‘I can’t describe it. It was a seizure.’ She left to ask the doctor. When she came back, she said, ‘They told me to tell you that you had a generalized tonic-clonic seizure.’ At that point, everything stopped. I thought, ‘How could I have a seizure? I’ve never had a neurologic problem or seizure in my life.’ Fast-forward from there, they put me in a CT scan, and they saw a tumor. They decided to send me to the hospital for more tests. I was in the hospital for three days, where they ran tests including continuous EEG monitoring and functional MRIs, all the things I knew about from my work as a neuropsychologist, treating people with brain disorders. None of it seemed real. Luckily, I had my laptop and lots of friends on speed dial to support me. Finally, they gave me a diagnosis. They told me it was a brain tumor. And that, given the characteristics, it was most likely a GBM, a, glioblastoma, which I knew to be the worst of the worst. None of it made sense. I thought, ‘brain tumors are rare and happen to other people, not me.’
BrainWise: What was the initial plan of treatment?
Dr. Spencer: I was able to get myself registered as a patient at MD Anderson Cancer Center at the University of Texas within 48 hours. In that respect, I felt incredibly lucky, because most people would not have had that opportunity. It all felt very surreal. I kept thinking, ‘I am the luckiest, unlucky person ever.’ It was hard to even conceive that something was wrong because I had no symptoms other than [being] in a complete state of shock. I had brain surgery two weeks later to remove the tumor. When the anesthesiologist, who assisted the surgery, asked me in pre-op, “Is this your first brain surgery?” I waited a good 10 seconds to respond because I thought he was joking and was waiting for him to laugh. ‘Who has more than one brain surgery?’ I thought. Now I know it is common for patients with GBM to have multiple surgeries. Luckily, I had an amazing neurosurgeon who was able to remove all the tumor from my right parietal lobe with no residual effects on my functioning other than intermittent numbness in my left hand. I then went on with my normal life. I started chemotherapy and radiation treatment. I continued to run my private practice and volunteer in the professional arena. I continued to see patients, even some patients with brain tumors who needed help with cognitive issues. It was a bit surreal to be a clinician and patient at the same time. I also gave a few talks on the emotional and cognitive effects of brain tumors and volunteered to be a mentor for other patients. This all happened during Covid-19, which added a layer of anxiety, since I was worried about getting sick.
BrainWise: How did the experience change over time?
Dr. Spencer: I was fatigued, as you can imagine, because I was going through chemo and radiation treatment. Then I [joined] a clinical trial, which was another form of chemo. I was always scared of having another seizure. After about nine months and following a mountain climbing trip with my family, I started to have some problems again with my left hand. My doctors thought I might be having a tumor recurrence. So, I went back in for a second surgery. It turned out that I did not have a recurrence; I was having necrosis, or damage from the prior radiation treatment. I fortunately went through that surgery well and with no residual problems. My good luck continued. I’m not sure if being a neuropsychologist helped or hindered my situation. I knew what to watch for and all the ways to keep my brain healthy. Over time, the radiation effects continued leading to headaches and a third surgery. I then went on medication to control the radiation necrosis that essentially caused me to have a small stroke, proving that the treatments can be as bad as the disease. I was lucky that my cognition and personality stayed intact, but I suffered sensory changes and weakness on the left side of my body I started going to physical and occupational therapy; [coincidentally] I did those treatments in the same place where I had completed my fellowship 20 years before.
BrainWise: What have the last six months been like?
Dr. Spencer: A few months ago, I started to have some problems with my vision, and I decided it was time to stop working, because I didn’t want to risk making a mistake. Since then, I’ve focused on my rehabilitation therapies. As you might imagine, I’m not the typical patient. As a neuropsychologist who has worked in rehab hospitals for 20 years, I am constantly pushing myself and thinking of ways to use the intact parts of my brain to compensate for my areas of weakness. I work closely with my therapists to set goals and make it a priority to stay active in my home and community. I love a challenge and urge my therapists to set harder goals for me. Over the last six months I’ve been doing volunteer and advocacy work for the National Brain Tumor Society and the American Brain Tumor Association. I serve as a mentor for other patients with GBM. I also serve as a patient advocate for research and clinical initiatives. That work has been incredibly fulfilling to me, and I hope it makes a difference for other patients on this crazy journey.
Medically, I just participated in a phase-one clinical trial, but I had to stop due to adverse side effects. There is no cure for GBM, so treatment is ongoing. Despite my feeling good, my last MRI was worrisome. So, my treatment team recommended a second round of radiation. From a functional standpoint, I still have problems with my left side. I can walk with a cane, but in the community, or for longer distances, I use a wheelchair, I have a home physical therapy program and participate in an open gym neurorecovery program to make sure I stay as strong and active as I can. Rehab has been my saving grace.
BrainWise: What have been the biggest challenges for you in enduring this disease?
Dr. Spencer: It’s been a unique experience going through this with the knowledge of a neuropsychologist. I have assessed myself through this entire journey. In the beginning, I gave myself the grooved pegboard test to [evaluate] fine motor dexterity in my hands, because my symptoms started in my left hand. Over time, I’ve been acutely aware of my memory and problem-solving skills to make sure my decision making is still sound. Each time I had surgery, I woke up and gave myself a memory test, which my neurosurgeon found humorous and advised me to stop doing. Now, I continue to stay focused on my cognition, but I also try to take care of my mental health because the ups and downs of this disease can be discouraging. I make sure to follow the counsel I gave my patients in the past about [getting] rest, cultivating mindfulness, and appreciating the little joys in life. I also try to keep a good sense of humor and frequently make jokes about how brain tumors mess with your head or how we should give our non-dominant hand more credit. After all, we need [those non-dominant hands] to scratch itches and hold our phone while texting!
Rehabilitation has been my passion in neuropsychology; the question I’ve asked for years is, ‘How do we help people with brain injuries get to as close to their everyday lives as possible, and help them integrate back into their communities, and their family roles?’ The difficult part of GBM is that the symptoms fluctuate. Just when you think you’re getting better, something else comes and pulls the rug out from under you. I’ve had to fight every step of the way. Something sets me back. Then I get better. Then something new happens. That has been a big challenge. Each time I’ve had a setback, I ask myself, ‘What can I do to get my brain working the way I want it to work again?’ In many ways I think of my journey like Sisyphus and his boulder—every time I think I’ve pushed the boulder to the top of the mountain, it falls back down, and I need to start over again.

BrainWise: How do you wrap your conscious mind around what you’ve been through?
Dr. Spencer: I’ve spent 20 years working with patients in my situation, so sometimes I’m my own therapist. In dark moments I tell myself, ‘What do you now need to do? You need to stay socially, cognitively, and physically active.’ I still want to live a meaningful life. And so, I have practiced what I preached to my patients for all those years. Even on the days when I feel discouraged or don’t want to do anything, I make myself reach out to friends, and make sure I’m doing things I care about, because I know that is the best thing that [one] can do for recovery and for the brain. I also still want to be part of the world. I am not sure what the alternative would be. I love hiking, so we bought a trail-friendly wheelchair. I love music, so I try not to miss my favorite bands when they’re in town for concerts.
BrainWise: How has your family responded to this diagnosis and the situation?
Dr. Spencer: My husband works from home now, and we have two teenage daughters. I don’t want to be a burden on my family. I want to be present and remain an active part of my family. At first, we just went through life as normal. We told [our girls] what was happening with me medically. For a long time, I didn’t say the word, ‘Glioblastoma,’ because I didn’t want them to look it up. Eventually, the stress of surgeries and treatments built. I encouraged them to ask questions, and I answered them. This is a shared experience. It isn’t something that is happening just to me. It is happening to the whole family. Like I said, we try to keep life as normal as possible, and I think they have adjusted well. Less than 24 hours after I got home from one of my surgeries, my daughter came down and asked me to order her stuff off Amazon. It was like, ‘Okay, I’m going to take that as a sign that they’re normal teenagers through this whole thing.’ We’re not hiding anything. Because there’s no way that you can. We’re going back and forth to the hospital all the time. We make sure they have support, that sure they spend time with their friends, and we keep the communication open.
BrainWise: How has the experience changed you as a neuropsychologist?
Dr. Spencer: I feel like I understand better when someone is sharing their experience as a brain injury patient. [Neuropsychologists are big on test scores, but] A person’s experience is more than just a test score. As a neuropsychologist, I was very focused on how our services improved patients’ lives, not just neuropsychology as a field, but where is the value that we bring to healthcare? And I think the value that we bring is this: How do we make patients’ lives still full and meaningful in the face of cognitive impairment? Because GBM affects the brain, it can affect the core of who you are and how you cope. As a neuropsychologist [now going through this as a patient], I worry, ‘What if this disease takes that away from me?’ It terrifies me to think, ‘What if I start to have significant cognitive impairment or personality changes?’ I’ve seen these changes in my patients and worked with their families.
When I talk with my doctors about my treatment plan, I’m always focused on those issues. I’ll ask them, ‘Okay, what is this going to do to my cognition?’ I always tell my neurosurgeon, ‘Thank you for sparing my frontal lobes, because that means I can now bug you with lots of questions.’ We regularly talk about brain regions and what my preferences are. I think that’s probably different from other patients, who may not be able to speak at that level of specificity. When I’m looking at my MRIs, I might say, ‘Oh, there’s the place where I lost my motor function,’ or, ‘I don’t want [the tumor] to move over here, because then it may affect my personality.’ Overall, my neuropsychology background allows me to advocate for myself in ways that other patients might not. It also makes the situation more terrifying because I know things that other patients may not know. Sometimes I think awareness is a blessing and a curse. Funny enough, the location of my tumor often affects people’s awareness, so they may not fully understand or be aware of their deficits. But my awareness has been quite good. There are some days that I ask, ‘Is [awareness] a good thing?’ Maybe it would be better to be a little bit blissfully ignorant.

BrainWise: What have you learned as a patient that you didn’t know before?
Dr. Spencer: Doctors need to see their patients as people. They shouldn’t make assumptions. Some doctors and health care providers treat you differently when they see you in a wheelchair and they see your diagnosis. They make assumptions. When you’re a clinician, you’re living in a bubble. I miss that bubble. I really do. I look at my doctors and my therapists, and I know they’re in a bubble. Being outside of that bubble, I often think about when I was in that bubble. I [think] I was a compassionate clinician. I remember many of my patients vividly. I wish I could be with some of them now. I would do some things differently. When I reflect, I really feel like I understand their experience better, having now gone through something similar myself.
BrainWise: As uncomfortable as it might be to discuss this, what is your prognosis?
Dr. Spencer: Generally, when people are diagnosed with a GBM, the average [prognosis] is eight to 12 months. For me, I’m close to 3 years since my diagnosis. It hasn’t been an easy three years but I’m here and continuing to find new meaning in life every day. I still think I’m one of the luckiest unlucky people ever. I’ve already thought, ‘If I start to have some deficits, how am I going to handle that?’ My answer: I’ll continue to work hard in rehab. And I’ll work through the fatigue. I’ll stay active and keep doing what I’ve been doing. I’ll just keep pushing the boulder, no matter how many times it might come back down the hill.









