Her plastic brain
In this personal essay, author Helen Santoro shares her experiences about life with a hole in her brain, and she details some of the ways in which her brain has adapted over time. Please be sure to check out our companion feature, a Q&A with Dr. Erin Bigler about neuroplasticity and adaptability of the brain, as well.
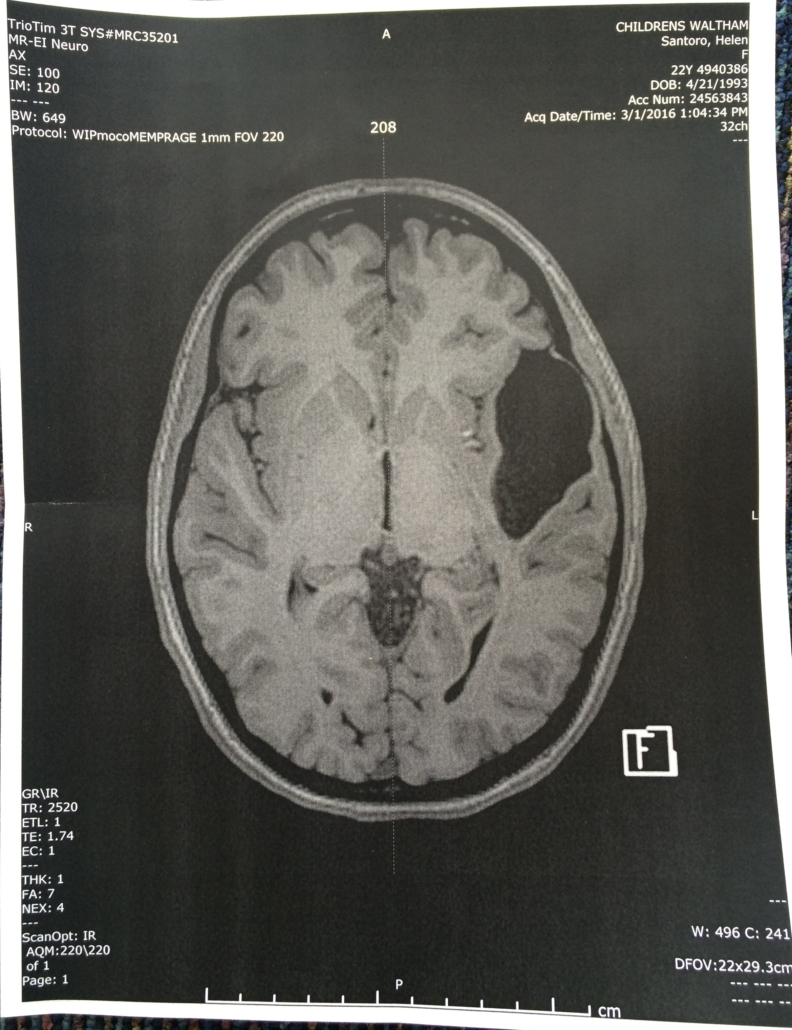
The first time I saw a picture of my brain at 22 years old, I gazed at a giant black hole where a chunk of brain tissue should have been.
I was in my boss’s office at a clinical research lab at Boston Children’s Hospital — my first job out of college. He slid a printout of a slice of my brain across the desk. The scan was taken a few weeks earlier when I hopped into the MRI machine to test a new scanning protocol. When I saw the picture, my eyes widened in astonishment.
Situated behind my left temple and eye socket was a gaping, black cavity that looked about six centimeters in length, the size of a dollar bill. The surrounding brain tissue was abnormally contorted and compressed, and the lesion — damaged or missing brain tissue — pushed up against the inside of my skull.
I had known since I was a teenager that I had a special brain. When I was born, doctors told my parents that I had a stroke in the uterus, otherwise known as a perinatal stroke. Consequently, I was missing my left temporal lobe, a region of the brain considered critical in language. My parents enrolled me in a study that tracked the developmental effects of perinatal strokes at New York University’s Langone Child Study Center from birth to 15 years old. I later wrote about it for The New York Times.
But I had never seen an image of my unusual brain. Not until my boss slid the picture across the desk.
Clearly, even with this hole in my brain, I can still write and talk — both are my personal and professional passions. The networks of neurons in my left temporal lobe have somehow reconfigured themselves. But scientists still don’t understand how this rewiring happened, or why my early-life stroke didn’t lead to the many developmental and cognitive issues about which doctors had warned my parents.
My life has been defined by the wonders of neural plasticity, but how and why my brain rewired the way it did is still a mystery. A mystery I face every single day.
The mysterious Tan
Almost everyone who has studied neuroscience or psychology knows about the French physician Pierre Paul Broca and the mysterious Patient “Tan.”
Tan wasn’t the patient’s real name. That was Monsieur Louis Victor Leborgne. Broca called his patient “Tan” because that’s the only word the adult Leborgne could say. One syllable: Tan. He usually uttered it twice in a row. Tan Tan.
It was a spring day in 1861 when Broca presented Patient Tan’s brain to his colleagues at a Société d’Anthropologie meeting in Paris. The talking point was whether or not mental functions — particularly language — are localized to certain areas of the brain. This question had been explored since ancient times, yet few had physically investigated the fast-decaying human brain.
That was until Leborgne came along. Leborgne was admitted to a hospital in Paris, and at age 51, was transferred to the surgical ward due to a gangrene infection in his leg. This is where he met Broca.
“This unfortunate man, unable to speak or to write with his paralyzed right hand was quite a difficult subject to study,” Broca jotted in his patient notes. “His general condition was furthermore so poor that it would have been cruel to torment him with over-long investigations.”
Leborgne died soon after the infection consumed his leg. Less than 24 hours later, Broca carefully cracked open Leborgne’s skull and examined his brain. Alongside a noticeable loss of tissue in parts of the left frontal and temporal lobes, Broca found a chicken-egg-shaped crater that was filled with fluid and located in the left hemisphere’s inferior frontal gyrus — a section of the brain located at the bottom of the frontal lobe that has been implicated in language comprehension and production.
The first time I heard about Leborgne, I was 17 years old and in my high school AP Psychology classroom. At the time, I had just uncovered details about my own medical history, specifically that I was missing a big section of my left hemisphere, though I still did not know where the hole was located or what it looked like.
Before this, I only knew that scientists were interested in my brain and that I was at risk of petit mal seizures — brief and sudden lapses of consciousness that cause people to stare blankly out into space for a few seconds. Consequently, I was on Topamax, an anti-seizure medication, for much of my childhood.
However, I was never convinced that I had seizures. At 12 years old, I decided to stop ingesting the little white pills and would hide them in the space between my bedframe and the wall. Nothing changed and I never had any seizures.
My mom was also skeptical about this diagnosis. I asked her if she recalls me ever having seizures. “No, never,” she responded immediately. Furthermore, she never knew that I stopped taking the Topamax.
Unusual symptoms
I never had seizures, but I have experienced other curious symptoms. Some of these come and go. Others are part of my everyday experience.
For instance, I struggle to see in the cold. Typically, I have normal vision. But when I am outside on a chilly day, it gradually worsens and eventually everything further away becomes an array of blurry colors. If I put on glasses during these periods, my vision is suddenly corrected.
One neurologist posited that my lesion, which presses up against the back of my left eye, may be constricting blood flow to the vessels that surround and fuel the optic nerve, a bundle of millions of nerve fibers that come out of the back of both eyeballs and relay messages to the brain. When it’s cold, blood vessels can constrict. Perhaps this narrowing of the vessels is exacerbated by my large lesion, thus impairing my vision. Another neurologist who I spoke to think this oddity is completely unrelated to my lesion.
Consequently, this odd symptom has been a constant companion — and puzzling mystery — throughout my entire life.
I also regularly struggle to recall words. For example, if I want to say “coral reef,” I can picture a coral reef and say words related to it, like “sea turtle” or “ocean.” I’ll also know the word starts with a c-like sound, but will only be able to recall random words like “cauliflower” or “Kraken.”
Sometimes, I can even be staring right at an object and will have no idea what it is called. This happened recently. I saw a safety pin and knew that it was an object that fastens two pieces of fabric together, but I could not conjure the words. It’s a very frustrating sensation, and one I wish I understood more.
Unraveling the research
Luckily, there has been a recent surge in research on the left hemisphere and language that may help make sense of these symptoms and how they’re connected to my unique brain development.
A study by researchers at Vanderbilt University in the journal Brain, for example, found that the location of a stroke in the left hemisphere impacts how well people recover from aphasia, or a disorder that impacts an individual’s ability to speak or understand language.
Scientists recruited 334 adults, 218 of which were experiencing aphasia who were followed for one year following their stroke. Those who had a lesion closer to the front of the brain recovered significantly better than patients who had brain damage in the region where the temporal and parietal lobes collide. This suggests that damage to some regions of the brain may have a greater impact on the language network — which encompasses the left temporal and frontal lobes, according to recent research — than others.
Aphasia impacts a third of adults following a stroke. Babies who suffer a perinatal stroke, on the other hand, are far less likely to experience aphasia, likely because the brain is remarkably plastic in newborns.
Additionally, both the left and right hemisphere appear to be equally involved in speech early in life, with language becoming more confined to the left hemisphere as people age, according to a 2020 study published in PNAS by researchers at Georgetown University and Children’s National Hospital in Washington, D.C. Additionally, in infants who had a left hemisphere perinatal stroke, the language network shifts over to the right hemisphere, based on a 2022 study published in PNAS.
Where we go from here
Before I can apply any of these findings to my own life, however, I must first answer if I had a perinatal stroke in the womb. It has been suggested by some doctors that the lesion in my brain is a large sac filled with spinal fluid, known as an arachnoid cyst. These cysts impact about 3% of all children and most are completely benign and never require any treatment. This April, I’m scheduled to see a neurologist to hopefully answer this question.
I am also participating in a study at the Massachusetts Institute of Technology to determine how damage to the brain impacts the language network. According to a preliminary analysis of my MRI scans taken last summer, I still process language using my left hemisphere. This is unlike another woman in the study who is also missing her left temporal lobe and now processes language using her right temporal and frontal lobes.
By understanding why my brain is missing so much tissue, I can better piece together how my language network adapted early in life. Maybe there was enough healthy tissue left over in my left hemisphere and the neuronal circuits that are typically in a left temporal lobe are all squished around the large hole. Maybe my language network moved to other parts of the brain like my left frontal lobe behind my forehead and parietal lobe underneath the crown of my skull, which is why I can still process language with relative ease.
There is also the question of the extent to which my condition is congenital, and whether other members of my family also are missing chunks of their brains. When I went to MIT to get my brain scanned, my mother also hopped in the MRI machine. Her brain was normal. My father has gotten his brain scanned many times and doesn’t have any noticeable irregularities. However, both of my brothers have never seen their brains, and researchers at MIT hope to scan both of them one day.
The other woman in the MIT study whose language network flipped over to her right hemisphere has a sister who is missing her right temporal lobe — and also lives a relatively normal life. Are there genetic factors that make people like me and this woman more susceptible to gaping cerebral cavities? Or is it all environmental, and something random happened during my fetal development or birth that caused my brain to develop the way it did?
Also, there factors that make some individuals’ brains more plastic than others?
I would also love to uncover why my vision is impaired in colder temperatures. I have no idea how, or if, this can be tested, and have yet to meet a researcher or neurologist who has ever heard of anyone else with this odd symptom.
My ability to understand my odd, plastic brain is entirely dependent on scientists’ ability to further decipher the complexities of neural plasticity. This will take years, as science is anything but quick. Regardless, I’m grateful that my brain can contribute to these discoveries and am excited to see what researchers uncover.
Check out our companion feature, a Q&A with Dr. Erin Bigler about neuroplasticity and adaptability of the brain.
Helen Santoro is a freelance writer.









